Sisters4Prevention Breast Cancer Stories and Survival
Since my diagnosis fourteen years ago, I have been dedicated to researching lifestyle changes and supporting clinical research to achieve the prevention of breast cancer. My goal is to raise awareness of the need for research funding for the primary prevention of women's cancers and to share information to help those facing this journey. My posts are educational and include my journey with bilateral breast cancer and my year of treatment including a double mastectomy and reconstruction. I have been a breast cancer advocate since 2010 and have served on panels at the department of defense breast cancer funding review programs. My website shares all the information I have collected and verified from long term survivors and medical evidence. I am not a medical professional, simply a teacher who hopes to make a difference by sharing information. I presently serve as one of three breast cancer advocates on the pending clinical trial under the direction of Dr. Vincent Tuohy at the Cleveland clinic to prevent the recurrence of triple negative breast cancer, the most lethal form of the disease began in the Fall of in 2021.I am a graduate of the National Breast Cancer Coalition's Project LEAD and have lobbied Congress for additional funds for prevention clinical trials for breast and ovarian cancers. In 2022, I was invited to be a Komen Advocate in Science. Stay tuned...
Sisters4Prevention Breast Cancer Stories and Survival
How Does Breast Cancer Evade the Immune System and How Does Chemotherapy Work
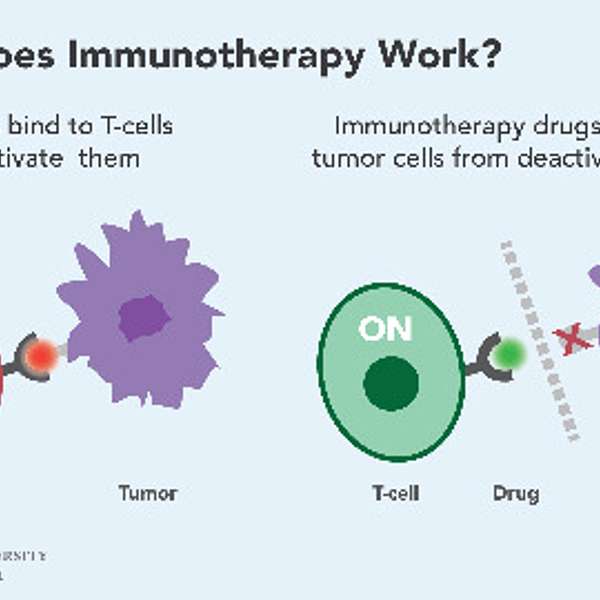
Our immune system is the “clean up crew” which constantly surveys for foreign invaders such as bacteria and viruses. These harmful substances are called antigens. Our Immune surveillance system identifies these invaders, marks them, and calls out the cavalry, the T cells, to destroy them. Macrophages are large white blood cells that are an important part of the immune response. The word macrophage literally means “big eater”. Its job is to clean our bodies of microscopic debris and invaders. It’s an ameba like cell that patrols out bodies and “eats“ intruders. Macrophages are able to pull apart enemy cell proteins and present (identify them) them to T cells as invaders. So what are T-cells? They are cells produced in the bone marrow which spend some time maturing and developing in an organ in the chest called the thymus—this is why they are labeled T-cells, which stands for thymus-derived cells. Once they are mature, T-cells are released into the blood and lymph nodes to start work. When a T cell is presented an invader by macrophages, it then will call out the cavalry (antibodies) to eliminate the diseased cell or invader. Specific types of T cells have particular functions, with helper cells activating other cells of the immune system while cytotoxic T cells directly kill foreign cells (cancers) and viruses. How cancer cells evade the immune system has puzzled scientists for decades. When cells are/or become abnormal, macrophages are supposed to consume and destroy them. So how do these diseased and abnormal cells evade this important checkpoint designed to keep us healthy? How are these cancer cells allowed to fly under the immune system’s radar? To put it in simple terms, cancer cells somehow send out a “don’t eat me” signal to macrophages by expressing certain proteins on their cell surfaces therefore, “disguising themselves” and tricking the macrophage. These surface proteins expressed by the cancer cell bond to other proteins on the surface of the macrophages paralyzing their ability to destroy or consume the cancer. The result is they are not presented to the T cells for an immune response. Since the immune system (T cell) does not identify the cancer cell as an enemy, it does not generate an immune response and allows other cells like it to continue undetected. So, if cancer can evade our brilliant immune system, how can chemotherapy identify and kill cancer cells? The honest answer is … it can’t. Chemotherapy works simply by killing cells that are rapidly dividing like cancer cells. Cancer cells need lots of glucose or sugar for the energy to divide. Every cell in your body uses blood sugar (glucose) for energy. But cancer cells use about 200 times more than normal cells. Chemotherapy is often administered in a glucose solution to entice cancer cells to absorb the treatment. Since they are hungrier and more aggressive, they “eat” the chemo first which is the objective of the treatment. The problem is that as well as killing cancer cells, chemotherapy also kills normal cells that are rapidly dividing like in the mouth, stomach and bowel (gut), skin, hair and bone marrow. Damage to these normal cells cause the side effects of chemotherapy. However, unlike cancer cells, normal cells can repair the damage and can recover. This is a total simplification of the complex immune response, but I hope it makes it understandable.
How Do Breast Tumors Evade the Immune System? - PHD Version by Dr. Vincent Tuohy, Immunologist. Please visit my website for the full transcript. https://www.sisters4prevention.com/post/how-does-breast-cancer-evade-the-immune-system-and-how-does-chemotherapy-work